Skin Grafting
History: In simple words it’s the transplantation of the skin and the tissues from a healthier side to the damaged one.
The Hindu Tilemaker Caste was the ones 2500-3000 years ago using this technique of skin transplanting, they use it to reshape the nose as a punishment. In late 19th century the more rapid techniques and procedures were used commonly by surgeons.
Skin Grafting only deals with the reconstruction regardless of the causes of damage.
Common Uses
- Mostly used after loss in full thickness skin and tissue burns to reconstruct the affected part.
- To cover up chronic ulcers, which are not healing up.
- After surgical removal of coetaneous malignancies.
Surgical Therapy
Numerous techniques and materials are used nowadays for reconstructing and harvesting skin grafts.
The procedures are categorized by surgeons majorly as:
- Split-thickness Skin Grafts (STSG)
- Full-thickness Skin Grafts (FTSG)
The method used, tools selection and procedures varies according to circumstances and surgeon’s choice.
Other methods of skin reconstruction are:
- Primary closure
- Second-intention healing
Skin grafting is done when the above mentioned methods are not convenient or unavailable.
In dermatological surgeries it is difficult to completely note down the history of patient. Some prior knowledge about medicines with anticoagulant properties, allergies, bleeding diatheses and wound healing extra are taken generally.
Split-thickness Skin Grafts
The defect is measured properly to rebuild the fault due to surgery. An STSG is chosed keenly to reconstruct the area. It’s good to have a stitch with purse-string around the selected area just to minimize its total size of donated graft.
The most suitable donor site for small area coverage are the buttock, thighs and arms, for repairing large areas more flat part is needed.
After the final selection of area, Anesthesia is given to the person donating graft. Free hand and Powered dermatomes are the instruments used for STSG harvest. Battery operated tools are required for larger areas, special practice is needed for harvesting such STSGs.
Sterile Sodium is used as a main Lubricant for chosen site of the donor. After cutting up the skin along with tissue, surgeon places it in a solution of sterile Sodium Chloride.
Trimming of the STSG is done after the graft is harvested just to fit in the donor. Overlapping is no problem as it can be finely treated by cutting. Surgeons fix up the graft using fat-absorbing sutures. Other option is to use basting stitches along with pressure dressings.
Wound on the skin of the donor should be treated properly. Healing time depends upon the thickness or depth of the wound. But normally 7-21 days are required for complete healing.
Full-thickness Skin Grafts:
These are mostly used to avoid several staged processes. Its known to have excellent results in one run. This procedure is generally selected when nearby tissues are inadequate or can’t be moved easily to the required area.
Locations that are convenient for FTSG are:
- Upper Eyelids
- Concha
- Nasal tip
- Forehead and inguinal fold skin
Every portion of the donor tissue should be preserved till end.
The procedure is almost same as for the STSG except that the donor and the recipient bed are prepared at the same time. No additional surgical tools are needed unlike STSG. The graft is refrigerated till the procedure ends completely. Shearing forces increases the vulnerability of the graft. So must be avoided till the wound heals completely.
General Postoperative Information:
After grafting when the patient comes for stitches removal, light pink outer look of grafted skin along with crispness at the borders of grafted skin is a good sign.
But the outer looks in such skin surgeries varies largely.
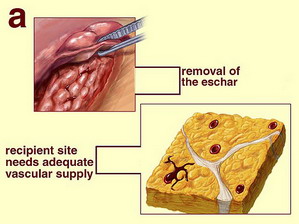
Grafted area is highly sensitive to sun burn and weak to resist trauma. The appearance of eschar partially or completely covering the grafted area is very alarming; it may results partial or total damage. And it can’t be diagnosed at early stage as it is a nature’s way of dressing any wound.
Infections, hematoma formation and contracture of graft are the challenges faced by Dermatologic Surgeon mostly. Good surgical procedures reduce the risk of infections and other complications. But if it happens oral antibiotics are given which covers staphylococcal and streptococcal. Diabetic patients are more prone to infections, studies showed.
Physical activities, like weight lifting, aerobics, etc. should be avoided at least for complete 2 weeks as it may cause seroma formation or Hematoma.
Chemical substances like Vitamin E, Aspirin, Coumadin, non steroidal anti-inflammatory drugs should be avoided before dermatological operations. And even afterwards for a week.
Any sort of mismatch can be corrected easily after main grafting procedures. Uneven surface can be smoothened by using laser technique afterwards. Administration carrying out a medical procedure not advisable.
STSGs are not recommended on areas where durability is the major requirement. Can’t be treated the sides where functionality is at risk through such grafting procedures.
FTSG given better apparent results as compared to STSG.
It is good to recall all the available possible techniques before choosing one. Drawbacks and significances should be considered according to the site selected for skin graft. For smaller defects its advisable to use the method of second-intention healing. A combination of STSG and second-intention healing may be used for better outcomes.
Any technique selected by physician should suite the requirements & budgets keeping in mind the case history of patient.